In Sync: Managing ADHD Across The Menstrual Cycle
Ever notice how some days you feel like you can conquer the world, and other times, you can't even conquer your laundry pile? 🙈Well, if you're juggling ADHD and the ups and downs of your menstrual cycle, you might be surprised to hear that this fluctuation in ADHD symptoms is often linked to where you're at with your period.
In this article, we'll look at:
- The science behind how ADHD symptoms can shift in intensity across the menstrual cycle.
- Actionable strategies for each phase of the menstrual cycle, from leveraging increased energy during the follicular phase to managing the challenges of PMS symptoms during the luteal and menstrual phases alongside ADHD.
- The small changes that can make a huge difference to support hormonal balance and ADHD management.
- How pharmacological treatments might help manage these fluctuations, including ADHD medication and hormonal therapies or birth control.
Ready to understand your body and tweak your cycle to keep things running smoothly?
Let's get into it! 💃
Note: We acknowledge that not all individuals who menstruate identify as women. Menstruation is a biological function primarily linked with women’s health, but it's important to recognize that not all women experience menstruation. This topic can be particularly complex for transgender and nonbinary individuals. We try to stick with language that focuses on biology rather than gender when discussing topics that relate to the body; however, we aim to use inclusive language as much as possible to ensure everyone in our community feels represented and respected. We know that people with ADHD already encounter stigmatization in many aspects of life, and we don't want to add to this further. 💕
How The Menstrual Cycle Effects ADHD
We already know that individuals assigned female at birth (AFAB) who have a diagnosis of ADHD face unique challenges. Our ADHD symptoms might not be as noticeable as those seen in men, leading to us being diagnosed later or sometimes not at all. We're also more prone to experiencing anxiety and depression alongside ADHD, and our compensatory strategies often mask our symptoms, leading to underrecognition and delayed support.
But what adds an even more complex layer to this is that our symptoms can get worse with hormonal changes, like during our menstrual cycle, pregnancy, or menopause.
But why is this? 🤔

Estrogen interacts with brain receptors that manage the release of dopamine, serotonin, and norepinephrine - neurotransmitters that play a pivotal role in mood regulation and attention processes. For individuals with ADHD, who typically have imbalances in these neurotransmitters, the hormonal fluctuations of reproductive steroids such as estrogens and progesterone can exacerbate ADHD symptoms even more than usual.
You Asked Us…
How is ADHD affected by hormones?
Hormonal fluctuations, especially in estrogen, can intensify ADHD symptoms. Estrogen impacts dopamine levels, influencing focus, mood, and cognitive function
The good news is that it's not all doom and gloom - by understanding the unique ways in which our symptoms change by where we're at in our cycle, we can better anticipate and manage our ADHD symptoms.
This awareness allows us to tailor our strategies and treatments, ensuring we can thrive through every phase of our cycle instead of constantly bouncing between 'the good' and 'bad' weeks.
Let's take a closer look at how these phases in the cycle might affect us, both positively and negatively. 👇
Post-Menstruation: The Follicular Phase
After your period ends, your body kicks off the journey towards ovulation, which begins with the follicular phase. During this phase, lasting 10 to 17 days, multiple follicles containing an immature egg start maturing, racing to become the dominant follicle that will release an egg during ovulation.

According to research, estrogen's activational effects on the brain can lead to a subtle improvement in ADHD symptoms during this phase. Essentially, as estrogen levels climb, there might be a positive impact on the brain's dopamine systems, suggesting a temporary easing of symptoms, which is usually a welcome relief after menstruation and what came before it. 😂
Some people find their symptoms are at their best during this phase, but others get the most relief during ovulation. 👇
Mid-Cycle: Ovulation
As we move into the heart of your menstrual cycle - ovulation - it's essential to note that this key event usually unfolds around the mid-point of the cycle.
While a standard 28-day cycle might see ovulation occurring between days 10 and 17, it's crucial to acknowledge the diversity in cycle lengths and timing of ovulation among individuals.
During this phase, estrogen reaches its peak, setting off a rapid release of Luteinizing Hormone (LH). This hormonal surge is the signal for the release of an egg, propelling it into the fallopian tube where it stands ready for the possibility of fertilization.

As estrogen and testosterone are at their highest during this time, there can be a rapid increase of positive effects for those of us living with ADHD. ✨
This includes:
- Enhanced Cognition: The peak in estrogen during ovulation can improve focus, memory, and cognitive flexibility. This boost can cause a noticeable increase in productivity, as tasks that might typically require a significant effort become easier to manage, meaning we're more able to multitask, organize our thoughts more clearly, and stay on track with our goals.
- Improved Emotional Wellbeing: We might experience reduced irritability and mood swings that often accompany ADHD, leading to smoother and more harmonious interactions with others and a more stable and positive mood overall. 🥰
- Increased Alertness and Energy: In contrast to the inattentiveness that individuals with ADHD often struggle with, this heightened state of awareness makes it easier to engage with the present moment, absorb new information, and respond more effectively to the surrounding environment. Additionally, this boost in energy levels during this time can help reduce fatigue and increase the desire for activities and socializing. 🍷
- Improved Sleep: Thanks to higher estrogen levels, sleep quality also tends to be better during this phase. Estrogen is known to have a positive effect on the brain's regulation of sleep cycles, promoting deeper and more restorative sleep. We may find it easier to fall asleep and stay asleep, experiencing fewer night-time awakenings and a more consistent sleep pattern. 😴
- Boost in Libido: Ovulation naturally increases libido due to the body's reproductive signaling. This heightened sexual desire can lead to a greater sense of connection and intimacy in personal relationships, potentially enriching emotional bonds. 💕
- Creativity Surge: The improved cognitive and emotional state during ovulation may also spark a surge in creativity; the increase in mental clarity and emotional wellbeing can inspire innovative thinking and artistic expression, allowing us to explore new ideas and creative projects. 🤩
For those of us managing ADHD, this period might feel like a brief hiatus from the usual challenges, with increased alertness and a more positive mood. During this time, you're likely more productive and efficient and less overwhelmed with everything that feels like the end of the world the week before your period.
Research also indicates that stimulant medications, like d-amphetamine, tend to have a more pronounced effect during the follicular phase of the menstrual cycle, which includes the ovulation period. In the study, participants reported feeling more energetic, euphoric, and intellectually efficient in response to the medication, suggesting estrogen may boost the subjective effects of stimulants, making them more effective during this part of the cycle. 💪
However, this can result in a bit of a shock to the system when we move into the next phase of the cycle - the luteal phase. 🙈
The Luteal Phase & The Premenstrual Phase
The luteal phase, a crucial part of the menstrual cycle, spans about 14 days following ovulation. During this phase, the body experiences a hormonal shift from high estrogen to increased progesterone levels, focusing on maintaining the uterine lining for potential embryo implantation - a process integral to reproductive health.
This period is not only marked by the body's preparation for pregnancy, with progesterone peaking a week after ovulation to support the uterine environment, but also signals the onset of the premenstrual phase for many.
In the days leading up to menstruation, commonly referred to as the premenstrual phase, individuals may experience symptoms associated with premenstrual syndrome (PMS), such as mood swings, bloating, and irritability. These symptoms are part of the body's response to the hormonal fluctuations occurring during the latter part of the luteal phase. During this time, research indicates that 90% of individuals (with or without ADHD) experience these symptoms, varying from mild to severe.
If fertilization doesn't occur, progesterone levels decline, leading to menstruation and the beginning of a new cycle. The sudden relief that many often feel from PMS symptoms when your period begins is usually caused by this sudden drop in progesterone. 🥵

For those with Attention Deficit Hyperactivity Disorder (ADHD), the luteal phase and the premenstrual phase often marks a period of heightened symptom severity, as this time sees a significant drop in estrogen, which directly impacts the brain's dopamine system.
The resulting hormonal fluctuations exacerbate ADHD symptoms in several ways.
Individuals may experience:
- Increased Inattentiveness
- Dramatic increases in forgetfulness
- 'Brain fog' and mental chaos
- More difficulties in planning, decision-making, and task management
- Emotional dysregulation, irritability, anxiety, and insecurity
- Low mood, crying spells and feelings of worthlessness
- Heightened sensitivity to environmental and sensory stimuli
- Increase in hyperactivity-impulsivity symptoms and r
- Physical clumsiness and chaotic behavior
- Increased risk of making frequent mistakes
- Reduced focus and productivity
- Exacerbated mood swings
- Loss of interest in daily activities
Over this time, the cumulative effect of these changes significantly disrupts daily life, work, education, and personal relationships for those that identify as women with ADHD, which can create an endless cycle of needing to overcompensate for the rest of the month.
Research findings suggest that the effectiveness of ADHD medications such as psychostimulants may be compromised during this time - particularly during the late luteal phase - due to these hormonal changes. Individuals often report that their usual medication dosages become less effective during this week, and studies indicate a decreased response to psychostimulant drugs as estrogen levels fall and progesterone levels rise. This has led to a call for personalized treatment adjustments, including potentially increasing medication dosages premenstrually to better manage symptoms. As with all medication adjustments, this should be done under medical supervision.
One silver lining of the luteal phase is that the symptom exacerbation (particularly impulsivity symptoms) during this phase often leads to the diagnosis of ADHD in teenage girls.
As their visibility of ADHD symptoms increases significantly during this time, healthcare professionals are more likely to identify and diagnose ADHD in these adolescent girls, who often slip between the cracks due to how their symptoms usually present.
You Asked Us…
Does low estrogen make ADHD worse?
Yes, low estrogen levels can worsen ADHD symptoms by affecting dopamine, a neurotransmitter critical for attention and emotional regulation.
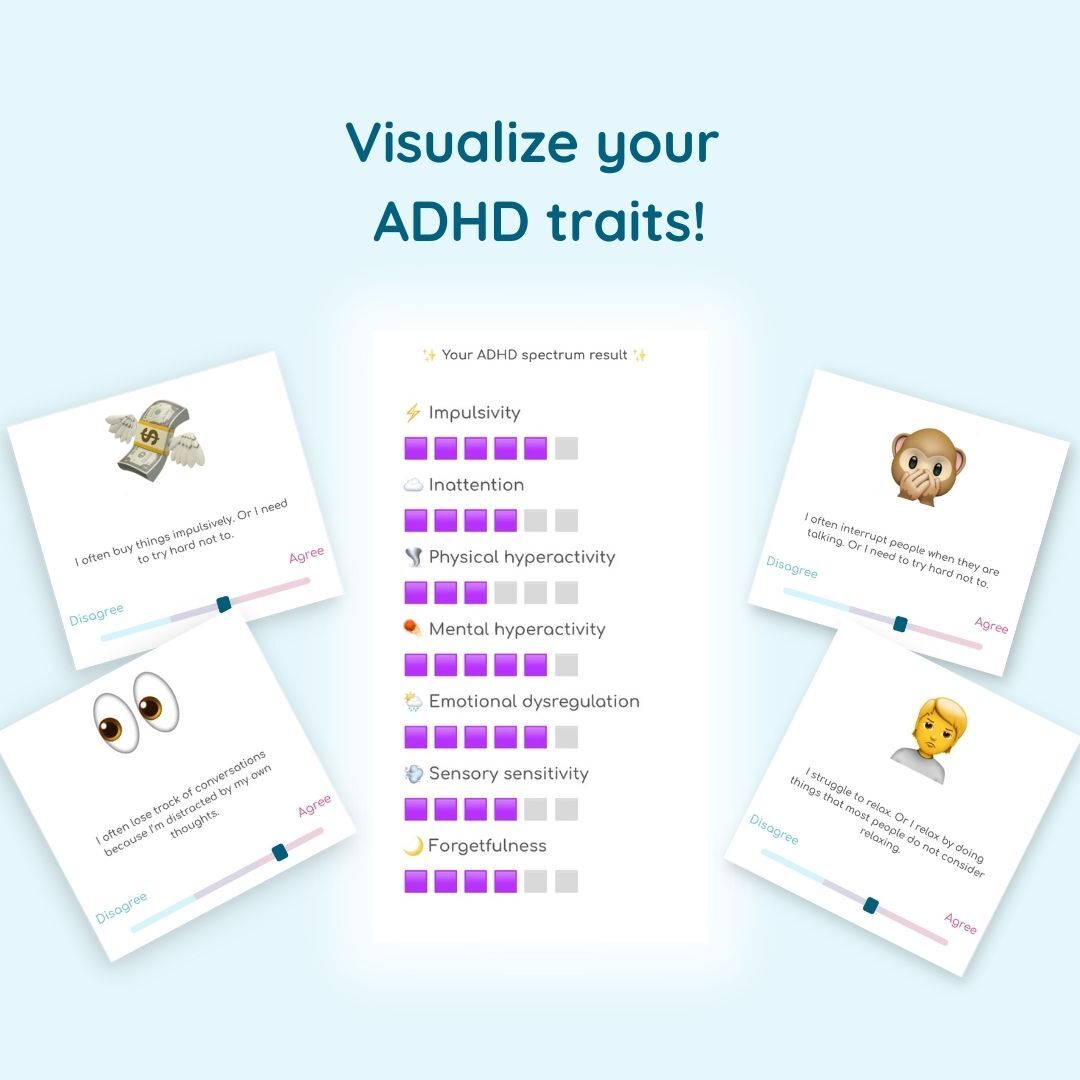
Take our fun online quiz to visualize your ADHD traits and learn more about your brain!
TAKE THE FREE TEST
Beyond The Menstrual Cycle
Estrogen impacts AFAB individuals and cisgender women with ADHD in more ways than just during the menstrual cycle, affecting overall reproductive health and potentially worsening ADHD symptoms. However, there's still a lack of detailed research and information available on this broader impact.
Here are just a few of the key ways in which estrogen affects these stages of the reproductive cycle.
PMDD
Premenstrual dysphoric disorder (PMDD) stands out from Premenstrual Syndrome (PMS) due to its intensity and the profound effect it has on individuals' lives. PMDD's symptoms go far beyond the discomfort of PMS, delving into severe mood swings, depression, anxiety, and significant physical symptoms around 1-2 weeks before menstruation. The severity of PMDD symptoms can drastically impact daily functioning and pose an increased risk of suicidal thoughts.
There is an undeniable link between PMDD and ADHD. A 2020 study revealed a notably higher occurrence of PMDD among AFAB individuals and cisgender women with ADHD compared to the general population, with 45.5% of those with ADHD diagnosed with PMDD, in contrast to 28.7% in the wider population.
Menopause
The decline in estrogen during perimenopause doesn't just signify a shift towards menopause; it also impacts other crucial neurotransmitters in the brain, notably dopamine and serotonin. Both play a pivotal role in managing ADHD symptoms, and their fluctuation during this period can exacerbate these symptoms significantly.
Cis-women with ADHD experience a significantly higher prevalence of symptoms associated with the climacteric phase, which includes menopause. This encompasses a range of symptoms such as anxiety, depression, sexual dysfunction, as well as the usual physical discomfort of menopause, illustrating the extensive impact hormonal changes have on mental health and daily functioning.
Research suggests that many cis-women report a worsening of their symptoms beginning around the age of 45; those who experienced more mild ADHD symptoms throughout their 20s and 30s may face a more challenging phase during perimenopause, where symptoms become more pronounced and more difficult to manage.
Pregnancy & Postpartum
Pregnancy and the postnatal period introduce significant hormonal changes that can affect the course of Attention Deficit Hyperactivity Disorder (ADHD). During pregnancy, the increase in estrogen levels can lead to a decrease in the most prominent ADHD symptoms. However, some pregnant individuals may experience heightened inattention symptoms as their focus shifts towards adapting to their new role as a parent.
In contrast, the postnatal period often sees a sharp decrease in estrogen levels, which can lead to reduced dopamine levels and, consequently, a depressive mood. This transition can exacerbate ADHD symptoms and introduce additional challenges for new parents, including the potential for increased vulnerability due to comorbid psychiatric disorders and low self-esteem.
Studies suggest that the overlap between ADHD symptoms and those of mental disorders such as depression and anxiety can lead to misdiagnosis and inappropriate treatment; many end up being treated for depression or other comorbid disorders without addressing the underlying ADHD.
What’s Medication Got to Do WIth It?
We've looked at how hormonal cycles and phases affect ADHD, and vice versa. But what about meds? Whether it's ADHD medication or birth control, any medication that impacts sex hormones can impact ADHD, due to the way hormones affect the brain.
Let’s dive into how these interactions play out. 👇
ADHD Medication & The Menstrual Cycle
Believe it or not, ADHD medication can actually mess with your period. For instance, Atomoxetine (Strattera), which isn't a stimulant but helps with ADHD symptoms, can lead to heavy flow, irregular cycles, or just painful cramps. Usually, these issues improve once your body gets used to the medication. Similarly, stimulants like Adderall and Ritalin can make cramps worse or cause heavier bleeding.
Oral Contraceptives and ADHD
On the flip side, the birth control you might be using to manage your periods or for other reasons can also have an impact on your ADHD. Since most birth control impacts estrogen levels, starting or changing birth control can make your ADHD symptoms fluctuate. For some, hormonal birth control can actually make things feel a bit more stable mood-wise, but this isn't true for everyone.
One 2022 study pointed out that, unfortunately, oral hormonal contraceptives might increase the already increased risk of depression for those of us with ADHD; researchers found that depression was six times higher for people with ADHD taking oral hormonal contraceptives compared to those without ADHD using the same type of birth control.
That said, if you're leaning towards non-oral hormonal contraceptives, like an implant or hormonal IUD, you might be in a slightly better spot. The study found that the depression risk for these methods was only moderately higher and more in line with folks without ADHD.
Hormonal Replacement Therapy & ADHD Symptoms
Transitioning into menopause with ADHD can be quite a journey, thanks to significant hormonal changes, particularly a decrease in estrogen during perimenopause. This stage, which typically stretches over four years, can lead to heightened ADHD symptoms. The decline in estrogen affects neurotransmitters like dopamine and serotonin.
However, there's a way through this. Guidelines suggest that medications such as Atomoxetine, Dexamphetamine, and Lisdexamfetamine remain effective for managing ADHD symptoms during menopause.
Lisdexamfetamine, for instance, is particularly helpful for improving cognitive functions affected by menopause, like memory and multitasking. If you notice your symptoms becoming more pronounced, talking to your doctor about adjusting the dosage of your current medication might help stabilize the hormonal fluctuations.
For those considering alternatives to stimulants, Hormone Replacement Therapy (HRT) offers a viable option by directly addressing the drop in estrogen levels. Often, a combination of medication or hormone therapy alongside psychological support provides the most comprehensive approach to navigating ADHD symptoms through menopause. 💕
You Asked Us…
Can HRT help with ADHD symptoms?
HRT can mitigate ADHD symptoms in individuals going through the menopause by stabilizing estrogen levels and supporting neurotransmitter balance.
Coping With Your Menstrual Cycle Phase-By-Phase
For those of us with ADHD, getting a handle on how our menstrual cycle affects our symptoms is key to keeping our day-to-day life on track without bouncing from crisis to calm throughout the month.
While sticking to the basics of self-care and wellness is a great start, there's room to get more specific with our strategies. To do this, tracking your cycle is essential; using period tracking apps and setting up alerts to give you a heads-up on symptom changes can be a lifesaver, letting you adjust your plans and routines for smoother sailing.
Here's how to adjust according to where you're at in your cycle. 👇
After Your Period (The Follicular Phase)
This phase is like hitting the reset button. 😎It's prime time for tidying up your space, indulging in some solid self-care, and reconnecting with friends. Pencil in those catch-ups, appointments, and any self-improvement activities for the next few weeks; you're most open and energetic now, perfect for expanding your world. In terms of exercise, post-period is your time to get back on track, so gradually amp up your workouts to match your increasing energy.
Leading Up To Ovulation
Now is the time to tackle those big to-dos - your energy and focus are on your side, so make the most of it. Connect with friends, go on adventures and enjoy those romantic connections and intimacy.
However, it’s also the best time to start planning for the luteal phase; move any big events and tricky decisions you might need to make to when you feel more on an even keel. Make sure all of your prescriptions are filled, especially if you need a slightly higher dose during the luteal phase.
In terms of relationships, keep your close ones in the loop about how your cycle affects you; this allows them to offer the right support when you need it. Remember, it's fine to begin gradually taking things down a notch and rely more on your support network as you move into the next phase.
Before Your Period (The Luteal Phase & Premenstrual Phase)
If your symptoms are particularly out of control during this time, it might be worth discussing your ADHD medication with a doctor to see if any tweaks are needed during this time to keep things effective all month. Overall, it’s essential to stress less, sleep well, and eat right to ease the hormonal rollercoaster's impact on your ADHD symptoms during this time. Accept that it's okay for this time to be difficult; remind yourself that even if everything feels too much now, it will pass very soon.
Menstrual Phase: Take It Easy
When you start your period, trim down your to-do list to just the essentials. Recognizing your need for more downtime during this phase can fend off overload and speed up recovery. Choosing foods that ease menstrual discomfort and steering clear of those that don't can make a big difference, while light exercise can help ease the aches and clear the fog. Adjust the intensity to what feels right for you, and don’t push yourself too hard as fatigue is more likely during this time.

Throughout Your Cycle
Taking care of your menstrual mental health goes beyond making adjustments during specific phases; it requires overall changes throughout the month. Regularly tracking your cycle, eating a balanced diet, staying active, and good sleep hygiene are your best bet to keep things regular and as predictable as possible. Supplements like omega-3s can also support your brain and hormonal health, whereas therapy and professional advice can build solid strategies for juggling ADHD and menstrual changes. Mixing these personalized strategies into your routine can help smooth out the menstrual cycle's ups and downs, supporting your wellbeing and productivity.
Key Takeaways
- Understanding the interplay between the menstrual cycle and ADHD is crucial for effective symptom management.
- Each phase of the menstrual cycle has distinct impacts on ADHD symptoms, including:
- Follicular Phase: Post-menstruation brings a surge in energy and focus. This is the best time to tackle big projects and engage in social activities.
- Ovulation: A peak in estrogen and testosterone can enhance cognitive functions and emotional well-being, offering a brief respite from ADHD challenges.
- Luteal Phase: Estrogen levels decline, leading to increased ADHD symptom severity, including inattentiveness, low mood, and hyperactivity-impulsivity.
- Menstrual Phase: Characterized by a need for rest and self-compassion, simplifying your schedule and focusing on manageable tasks.
- Individual experiences can vary greatly; some individuals with ADHD might find that their symptoms align closely with these patterns, while others may experience different effects or find that their symptoms don't closely follow their menstrual cycle.
- Beyond the menstrual cycle, conditions such as PMDD or reproductive phases such as pregnancy, postpartum and menopause, significantly intersect with ADHD. It's essential to take a holistic approach to treating ADHD during these times.
- Medications, including stimulants, birth control, and HRT, play an important role in managing ADHD symptoms but may require adjustments to address hormonal changes effectively.
With all these insights, you've got what it takes to tackle ADHD head-on, regardless of where you're at in your cycle. Remember, cycle syncing and crafting strategies that speak to you personally can make a huge difference. So, let's not just survive our period but learn to ride those hormonal waves that usually overwhelm us. 🌊
By syncing our strategies with our cycle, we can take charge and thrive every day of the month. 💪
What’s Next?
Learn more about the increased ADHD symptoms you might experience across the menstrual cycle in these related articles. 👇
A Deep Dive Into The Impulsive Side of Adult ADHD
Why Do People With ADHD Make Careless Mistakes?
The Emotional Rollercoaster of ADHD and Chronic Irritability
Visualize and assess 25 ADHD traits and understand how they affect your life.
Learn more-2.png)
Frequently Asked Questions (FAQs)
What are the hidden struggles of a woman with ADHD?
Those that identify as women with ADHD often face challenges that go unnoticed by others. These include managing the variability of symptoms across the menstrual cycle, where hormonal fluctuations can intensify ADHD symptoms. They might also struggle with societal expectations around organization and multitasking, where they may need more support. The interplay between ADHD and other mental health conditions like anxiety and depression, which are more prevalent in those assigned female at birth, adds another layer of complexity to their daily lives.
How does ADHD manifest in females?
ADHD in females often presents differently than in males, leading to underdiagnosis. Females are more likely to exhibit inattentive symptoms, such as difficulty maintaining focus, disorganization, and being easily distracted. These symptoms can be more subtle and internalized, making them less visible to others. Females with ADHD might also experience strong emotional reactions and sensitivity to rejection, adding to the challenge of managing everyday stressors.
Why is it harder to diagnose females with ADHD?
Diagnosing ADHD in those AFAB and women is challenging for several reasons, including: The presentation of ADHD symptoms can be less overt in females, often due to the predominance of inattentive symptoms rather than hyperactive or impulsive behaviors. There is a lack of awareness and understanding of how ADHD manifests in females, among both the public and healthcare professionals. Symptoms of ADHD in females are frequently mistaken for or masked by co-occurring conditions like anxiety, depression, and borderline personality disorder. This often leads to misdiagnosis or delayed diagnosis. The impact of the menstrual cycle on ADHD symptoms complicates the diagnosis process. Fluctuating hormone levels throughout the cycle can influence the severity and presentation of symptoms.

.png)